Outcomes in most areas of healthcare have improved dramatically over the last 50 years. For example, a 35-year-old woman diagnosed with adult lymphoblastic leukemia (ALL) in the 1980s had only a 24% chance of living for another five years. Over the next thirty years, the five-year survival rate for such a woman more than doubled to 59%:
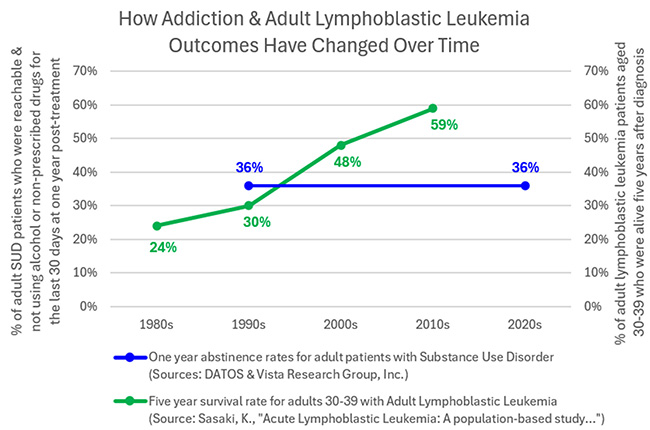
Unfortunately, we haven’t seen a similar improvement in the recovery rate of patients following addiction treatment. In 1993, the federally-funded Drug Abuse Treatment Outcomes Study (DATOS) found that one year after treatment, 36% of SUD patients were reachable and had not used alcohol or non-prescribed drugs during the last 30 days. Thirty years later, Vista Research Group’s one year abstinence rate for 22,742 addiction treatment patients is the same 36%.
Why have cancer survival rates improved
dramatically while addiction recovery
rates have stagnated?
For one simple reason -- far more practical research has been done to help patients recover from cancer than from addiction.
Since 1973, the SEER Registry has been collecting data on cancer diagnoses, treatment, and outcomes for millions of Americans. During this time, we’ve also invested billions of dollars in cancer-related clinical trials. An ever-growing body of real world data is accessible to researchers who are using it to make cancer treatment more effective.
If I were diagnosed with ALL today, my doctor would begin with blood tests and a bone marrow biopsy to identify chromosomal abnormalities and genetic mutations in my DNA. Based on those results, she would then select the chemotherapy drugs and targeted therapies most likely to be effective for my specific subtype of leukemia.
Let’s contrast this with what happens if I need treatment for addiction -- most likely, I will receive whatever type of treatment is offered by the rehab or MAT clinic I walk into first.
Hmmm. Despite the fact that the 20 million+ Americans struggling with addiction today is almost 500 times larger than the 44,000 people with ALL, we haven’t done the basic research necessary to predict what type of treatment is more likely to be effective for a specific individual than another.
Conquer Addiction’s Million Lives Initiative aims to change this with two innovative research projects. First, we intend to expand Vista Research Group’s comparative outcomes research to MAT centers so we can identify the drug use history, demographic and psychographic factors that make one type of treatment more effective for a person than another. Secondly, we are creating a de-identified national claims registry of addiction treatment patients that will allow us to identify the treatment providers and payers with the best recovery rates across the United States.
What factors predict whether a medication
is likely to help or hinder a patient’s recovery?
SUD medication can be a very effective recovery tool. Vista’s research shows that patients with Alcohol Use Disorder who leave treatment on Vivitrol are 26% more likely to be in recovery one year later than patients who leave treatment without medication. However, this doesn’t mean that everyone with Alcohol Use Disorder should be on Vivitrol. There are undoubtedly other factors that influence how likely Vivitrol is to help a specific individual recover.
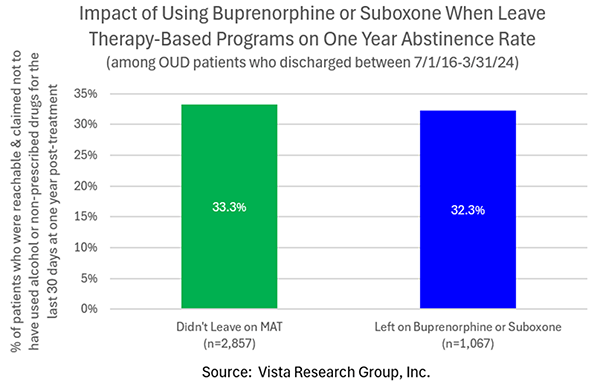
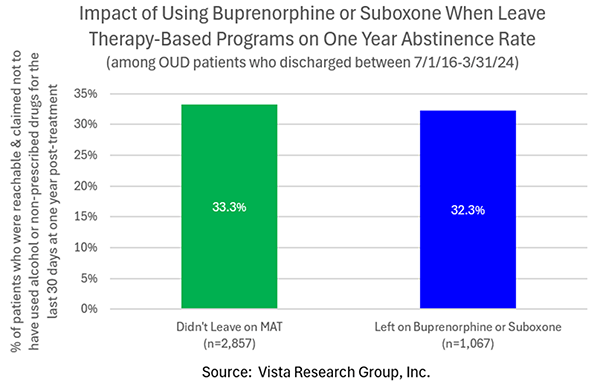
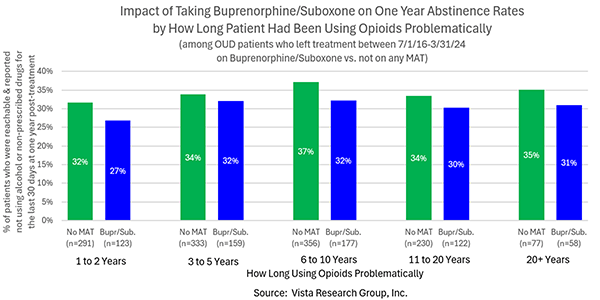
Digging into Vista’s results for Opioid Use Disorder (OUD) patients who start taking buprenorphine or Suboxone helps illustrate this point. Contrary to common belief, Vista’s research does not support that OUD patients in short-term, therapy-based treatment are more likely to recover if they take buprenorphine or Suboxone. In fact, while not statistically significant, leaving treatment on buprenorphine or Suboxone may actually hurt the likelihood of recovery for some patients:
Buprenorphine/Suboxone clearly helps some OUD patients, however. One of the few significant findings (p=.05) in our early research is that individuals who’ve been using opioids problematically for only 1-3 months have better outcomes on buprenorphine/Suboxone than if they receive therapy alone. These medications also appear to help patients in denial that their opioid use is a problem, although this difference is not statistically significant:
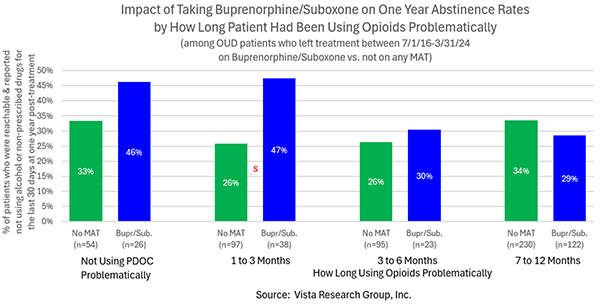
As the length of time someone has been using opioids problematically increases, the advantage of adding Buprenorphine/Suboxone on top of therapeutic treatment seems to disappear:
There are dozens of other factors besides length of problematic use that may affect the type of treatment most likely to be effective for an individual, such as their primary drug of choice and mode of usage, previous experience with a medication, age, gender, the existence and severity of co-occurring disorders, number of previous treatment episodes, whether they are in stable housing or living on the streets, etc. To ferret out the impact of all the various factors, we need comprehensive outcomes research on large numbers of patients.
Fortunately, Vista’s research has collected a tremendous amount of information on over 100,000 SUD patients attending a wide variety of short-term, therapy-based centers. To avoid basing our conclusions on data collected solely at therapy-based treatment centers, Vista has invested several years in creating comparative outcomes research for MAT centers.
To cover the entire spectrum of treatment, we also need outcomes research on patients
attending medication-assisted treatment centers
To this end, the second pillar of Conquer Addiction’s Million Lives Initiative is to raise the funding to follow up with 25,000 patients one, six and twelve months after they leave MAT centers to learn if they're meeting their self-defined drug/alcohol usage goals or have returned to active addiction.
This data will be combined with the post-treatment data Vista has collected to date on 23,000+ patients attending therapy-based centers to start predicting the type of treatment most likely to be effective for a patient based on their drug use history and demographic and psychographic characteristics.
By helping people predict the type of treatment that is most likely to be effective for them and then steering them to particularly effective treatment centers of that type through the national claims registry results, we believe we can help one million more Americans recover by 2030.
Interested in Helping to Transform Addiction Treatment?
Conquer Addiction is creating an Advisory Board for the Million Lives Initiative with providers, payers, funders, researchers and patient representatives to help us think through the important questions related to this project. If you’re interested in being involved in this advisory group, please reach out to Conquer Addiction with a short summary of your qualifications. Our first advisory board meeting will be on May 14th.






